
:max_bytes(150000):strip_icc()/GettyImages-200328303-031-5716defe3df78c3fa2e69694.jpg)
Clearly an abnormality in any of these systems will direct any further investigation and may lead to the diagnosis. otomastoiditis, tumours, cholesteatoma)īilateral peripheral vestibulopathy (if asymmetric)Ī patient with dizziness requires a thorough neurological, otological and cardiovascular examination, including supine and upright blood pressure measurements, particularly if the cause of the dizziness is not apparent from the history. Perilymph fistula/superior semicircular canal dehiscence Vertebro-basilar transient ischaemic attack/stroke Vestibular neuritis/labyrinthitis (acute unilateral peripheral vestibulopathy)
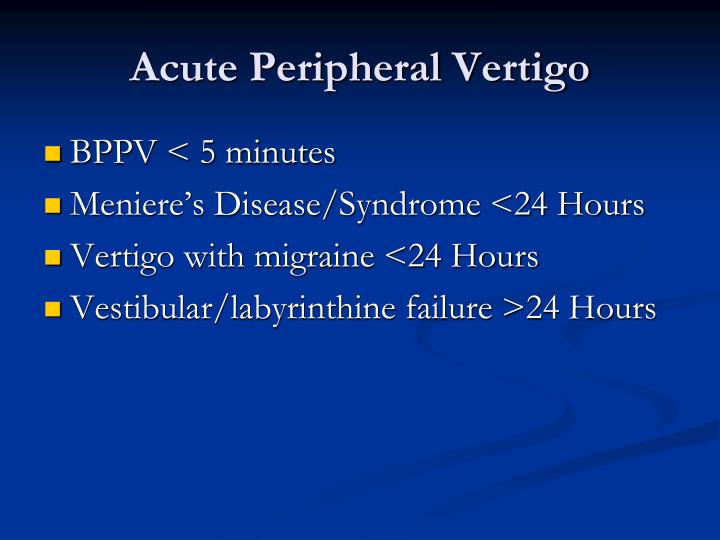
Hyperventilation may provoke or aggravate psychogenic dizziness, however it may also provoke vertigo from brainstem demyelination or an Arnold-Chiari malformation. For example, a change of head position may provoke benign positional vertigo, noise-induced vertigo (Tullio phenomenon) occurs in superior semicircular canal dehiscence, and pressure-induced vertigo (valsalva, straining, exercise) suggests a perilymph fistula. The circumstances that provoke the symptom of vertigo may provide important clues to possible causes. The patient's cardiovascular risk profile may raise the possibility of vascular vertigo. A history of migraine-like headaches may suggest migraine-associated vertigo, while a recent head injury may suggest a variety of different mechanisms of vertigo. The patient's medical history may reveal clues to potential causes of vertigo. Vertigo lasts less than one minute in benign positional vertigo, minutes in transient ischaemic attacks, minutes to hours in migraine and Ménière's syndrome and for more than 24 hours in vestibular neuronitis or posterior circulation stroke. The temporal profile of vertigo is important in analysing the patient's symptoms. For example, symptoms such as deafness, tinnitus and aural fullness or pressure might suggest a labyrinthine cause, whereas symptoms such as headache, diplopia, facial/limb paraesthesiae, weakness or clumsiness, dysarthria or dysphagia might suggest a neurological cause. The occurrence of associated symptoms may help localise the origin of the vertigo. Both the clinician and the patient want to rule out a serious cause, but localising the source of vertigo may be difficult. Central vestibular disorders include brainstem lesions and multiple sclerosis. If the patient has vertigo, is it peripheral or central in origin?Īlthough recurrent isolated vertigo is usually peripheral and benign, this is not always the case.

The dizziness occurs either through postural hypotension or direct effects on the central or peripheral vestibular system.
Dizziness which precedes a blackout or near blackout will usually indicate a syncopal/presyncopal disorder which requires a different approach.ĭrugs which can cause dizziness include antihypertensives, anticonvulsants, antidepressants and sedatives. The dizziness of benign positional vertigo may be provoked by specific positional manoeuvres while dizziness which is unaltered between resting and moving about is usually non-vestibular in origin. Its many causes (Table 1) may be central or peripheral. Is the dizziness of vestibular origin or non-vestibular origin?ĭizziness of vestibular origin (vertigo) is usually provoked or aggravated by movement and improved or relieved by rest (sitting or lying down). A framework of questions in the clinician's mind will serve as a guide in analysing the patient's complaint.


 0 kommentar(er)
0 kommentar(er)
